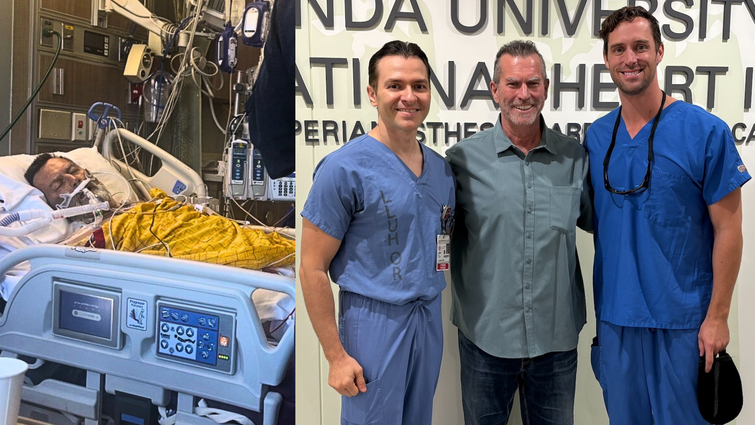
Heart failure patient Stephen Schuh returned to Loma Linda University Health recently to thank the team who cared for him including Dr. Amr Mohsen (left) and Dr. Jason Hoff (right). Just a few months earlier, he was in a hospital bed and in critical condition.
When 62-year-old Stephen Schuh awoke in a hospital bed surrounded by family, a priest, and the sound of life-support machines, he believed he was experiencing his final moments. His heart valve had failed. His liver and kidneys had shut down. His skin had turned a deep shade of yellow. Hours earlier, he had been airlifted to Loma Linda University Medical Center in cardiogenic shock after coding for several minutes at a nearby hospital.
A sudden collapse
For months, Schuh had brushed off growing fatigue and shortness of breath. A trip to Florida made the symptoms impossible to ignore when simply kicking a ball with his nephew left him breathless. A family member in healthcare urged him to get his decade-old surgical aortic valve evaluated. Before he could complete pre-operative testing for open-heart surgery, his condition rapidly deteriorated.
By June 2025, his heart rate was climbing uncontrollably. Days later, his valve stopped working entirely, sending him into cardiac arrest. Doctors at a nearby hospital stabilized him but told his family they had reached the limits of what they could do. His only chance was an emergency transfer to Loma Linda University Health.
When Schuh arrived, structural interventional cardiologist Jason Hoff, MD, immediately recognized how critical his condition was.
“He was as sick as they come,” Hoff said. “His skin was bright yellow from shock, his kidneys had shut down, and he was dying right in front of us.”
Within minutes, the Loma Linda University cardiogenic shock team mobilized — a high-acuity, multidisciplinary response only available at a few centers in the region. Schuh was placed on full mechanical circulatory support, including extracorporeal membrane oxygenation (ECMO) to take over the work of his heart and lungs, and an Impella pump placed minimally invasively, to maintain forward blood flow.
“He needed everything — ECMO, Impella, the shock team, the structural heart team,” Hoff said. “If even one of those pieces hadn’t been available at that exact moment, he wouldn’t have survived.”
A last-resort option
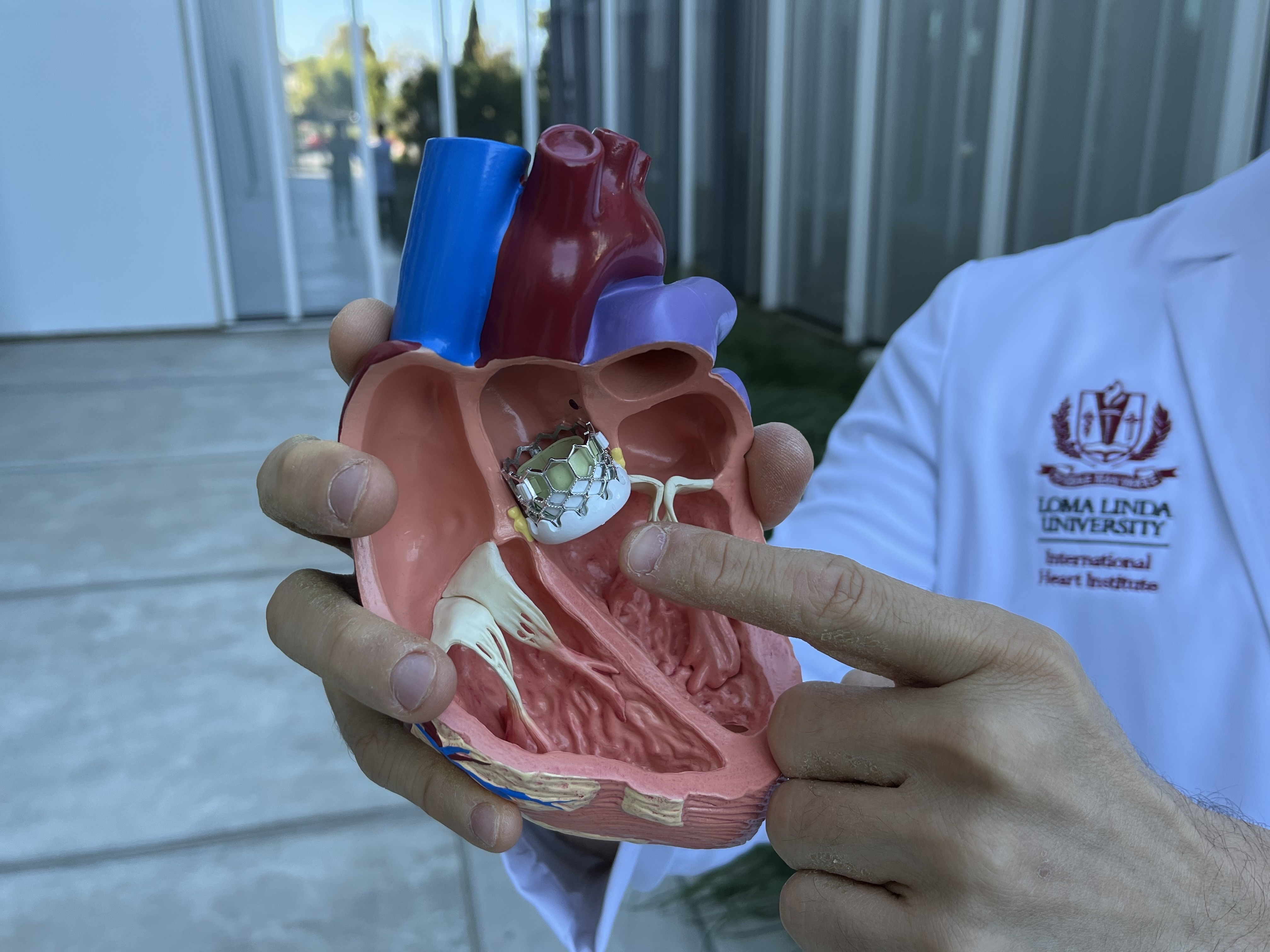
Once stabilized, the structural heart team including Hoff and Amr Mohsen, MD, performed a last-resort option: a high-risk valve-in-valve transcatheter aortic valve replacement (TAVR). Instead of opening the chest, they implanted a new valve inside the failed one through a minimally invasive approach, an advanced procedure rarely attempted in a patient this unstable.
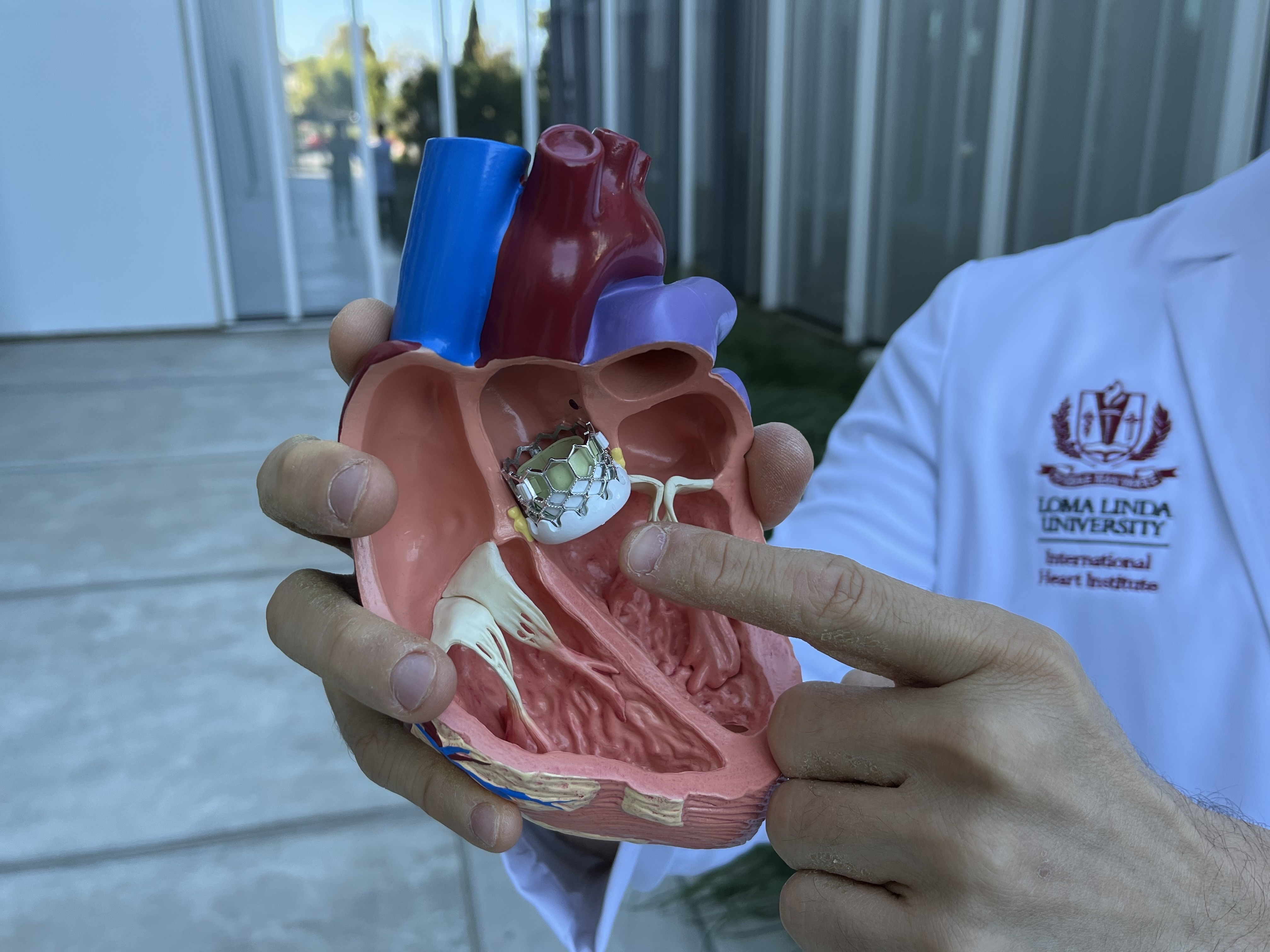
Dr. Amr Mohsen points to the transcatheter aortic valve replacement on a 3D model of a human heart. This TAVR valve was placed in Schuh's heart to restore blood flow and keep him alive.
“We brought him to the cardiac cath lab on full ECMO and Impella support,” Hoff said. “Most centers don’t attempt TAVR in patients this ill, but giving his heart a new valve immediately was the only chance he had.”
Schuh vividly remembers the moment before surgery. Surrounded by family, he watched as Hoff paused and asked to pray with them. “That moment gave me hope,” Schuh recalled. “I knew I was going to fight.”
The procedure was successful, and the turnaround was immediate. As soon as the new valve was implanted, Schuh’s blood pressure improved and his heart began to strengthen.
Over the next several days, his recovery continued. He walked out of the hospital just three weeks after arriving on life support. Although he required dialysis for several months, his kidneys steadily improved. Recently, his care team confirmed his kidneys had recovered enough to stop dialysis.
Hoff calls Schuh’s progress extraordinary, noting he was among the sickest patients the team has seen fully recover. He credits Schuh’s determination and the collaborative work of multiple specialty teams for the outcome.
Back on his feet
Schuh returned to Loma Linda University Health recently to thank the staff who cared for him. Healthy and steady on his feet, he greeted physicians, nurses, and therapists who were stunned by how different he looked from the critically ill patient they remembered.
“Seeing him walk in looking so healthy is the most rewarding part of what we do,” Hoff said.
Today, Schuh is back home with his wife of 31 years, children, and grandsons. He has made significant lifestyle changes such as adopting a heart-healthy diet, eliminating alcohol, prioritizing sleep, and embracing a more intentional approach to wellness. He sees the experience as a second chance.
He hopes others facing similar diagnoses trust their care teams and remain committed to recovery. He urges others to follow medical guidance closely and keep fighting because the alternative for him was death.

Schuh returned to Loma Linda University Health to thank the teams who cared for him during his time in the hospital. Just a few months before his skin complexion had turned yellow from his kidneys shutting down.
What's possible with advanced heart care
Schuh’s story highlights the advanced capabilities of Loma Linda University Health’s Structural and Valvular Heart Disease Program and its multidisciplinary model. Cutting-edge technology, rapid response, and expert collaboration aligned at the exact moment he needed it.
“This is exactly why programs like ours exist,” Hoff said. “This kind of outcome is what we strive for.”
If you or a loved one has been diagnosed with a heart valve or structural heart condition, our team is here to provide expertise, compassion, and advanced cardiovascular care. Make an appointment today.



