
Gastric sleeve surgery can result in weight loss of up to 80% of excess body weight
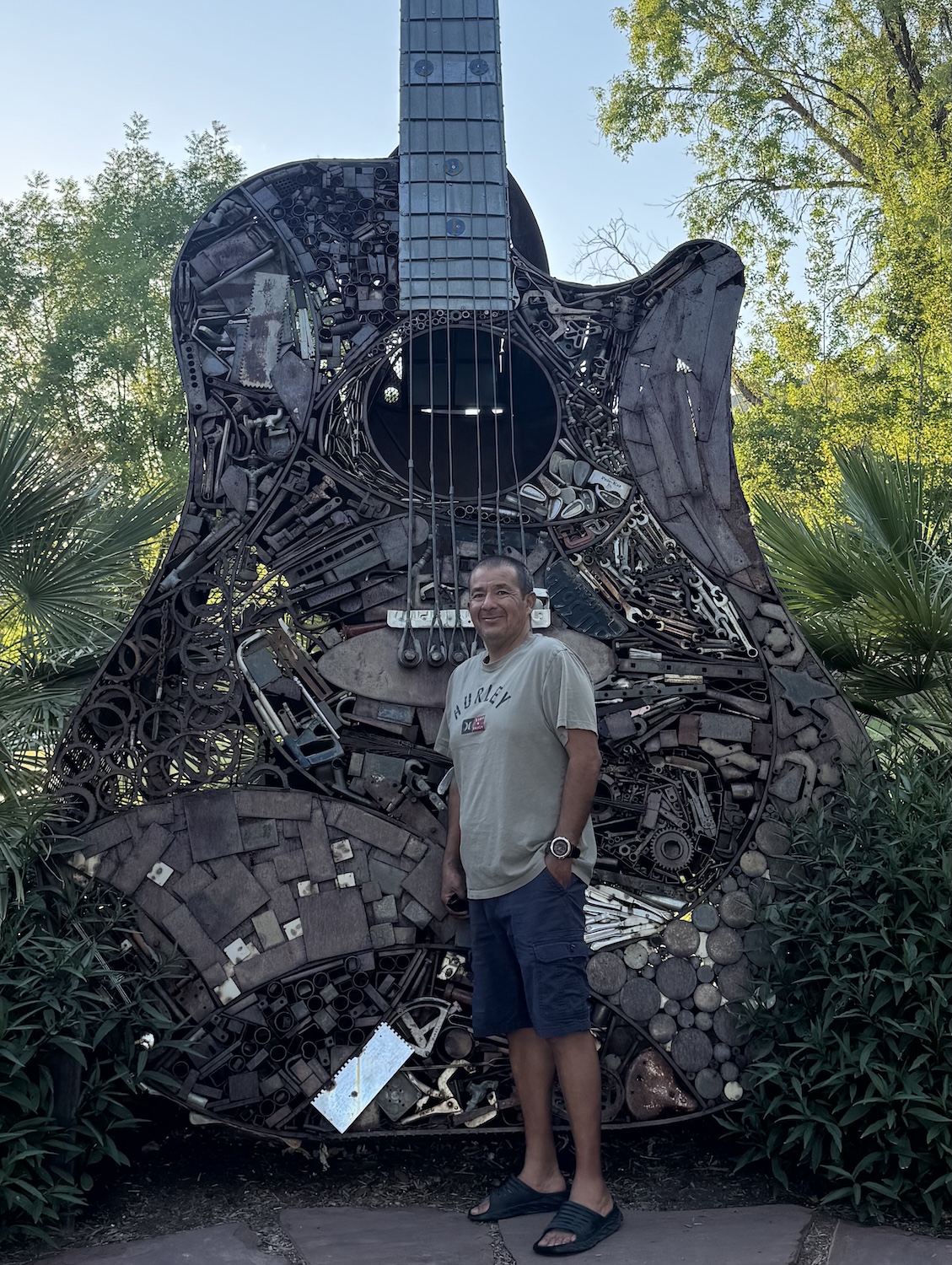
At his highest weight, Jose Angel Gonzalez weighed 250 pounds and faced several health challenges, including chronic sleep apnea, prediabetes, and high cholesterol. As a truck driver, Gonzalez was used to spending his days sitting behind the wheel with limited access to healthy foods.
Although he tried several times to lose weight through various weight loss medications, as soon as he stopped the medicine, the weight would come back.
“For me, medication wasn’t a permanent solution,” Gonzalez said of his frustration with temporary success. And as a husband, Gonzalez didn’t like seeing how worried his wife was about his declining health.
Determined to lose weight and get his health back, Gonzalez learned about various bariatric surgeries and found the gastric sleeve particularly interesting.
After checking his insurance options, Gonzalez learned he qualified for surgery through Loma Linda University Health’s Weight Loss and Metabolic Surgery Program.
Within a year, he underwent a successful gastric sleeve procedure performed by Keith Scharf, DO, FACS, FASMBS, Director of Bariatric Surgery at Loma Linda University Health.
This surgery not only changed his life but also potentially saved it.
Preparing for surgery
Before undergoing surgery, Gonzalez participated in a structured, comprehensive bariatric program that included nutrition classes, consultations with dietitians, and lifestyle education.
“I learned a lot,” Gonzalez said. “The classes helped me understand how my life would change after surgery, especially my diet.”
The importance of these mandatory classes is not just to prep a patient for surgery, but also to help shift their mindset for life after weight loss. Scharf says that without making lifestyle changes, long-term success becomes much harder.
“For patients progressing through the program, having a tangible goal can be incredibly motivating,” Scharf says. “As they work with our dietitians and mental health providers, they start identifying what needs to change in their routines for lasting success.”
Surgery day: sleeve gastrectomy
After completing educational classes and prep for surgery, Gonzalez underwent a sleeve gastrectomy, often called a gastric sleeve. This procedure is a popular one-hour surgery that requires just one night in the hospital.
“The surgery focuses solely on the stomach,” Scharf explains. “We staple and remove about 80 to 85 percent of the stomach using minimally invasive techniques, either laparoscopic or robotic, through several small incisions.”
The minimally invasive nature of the procedure allowed Gonzalez to get up and walk shortly after surgery — and the best part was that he experienced no pain.
Adjusting to a new diet
For the first several weeks, Gonzalez focused on walking daily, staying active, and following his liquid and soft–food diet.
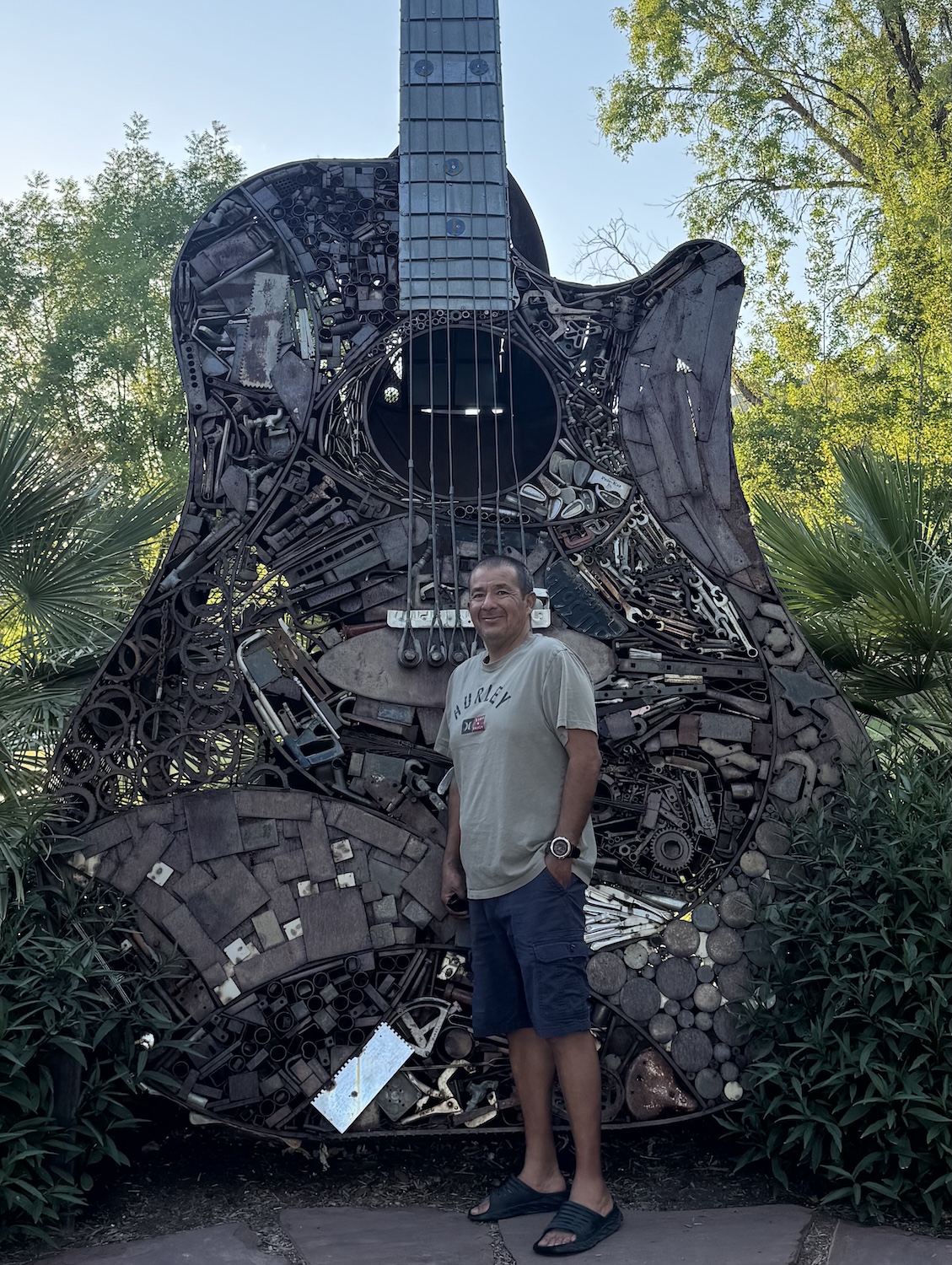
Gonzalez lost approximately 100 pounds after his gastric sleeve procedure
“We start patients on a clear liquid diet for about 24 hours while they’re still in the hospital,” Scharf explains. “Once they go home, they begin a full liquid diet for two weeks, then transition to a pureed consistency diet. After two weeks on purees, patients move on to soft foods, and then gradually progress to solid foods around the six-week mark.”
The main reason for this diet progression is to help patients learn how to eat again. With gastric sleeves, the sense of fullness and even taste can change dramatically after surgery. Eating something too heavy too soon can cause food to get stuck, nausea, vomiting, and chest pressure.
Life after weight loss
During this time, Gonzalez began to see the majority of his weight loss.
“The first four weeks were when I lost the most weight,” he said. “The drop was drastic.”
But beyond the weight loss, Gonzalez was determined to never return to his old eating habits, a success he credits not only to the classes he took through the bariatrics program, but also to his wife.
“Because I’m a truck driver, I used to buy a lot of fast food on the road, but not anymore,” he says. “My wife prepares my meals, which helps me stay on track. She is my biggest support.”
Within the first six months, Gonzalez lost about 100 pounds. In the seven years since his surgery, his weight has fluctuated within a healthy range, and he has maintained much of his weight loss.
“I maybe gained 18 pounds over the years, but I know how to manage it,” he said.
More importantly, the weight loss stabilized his health, his cholesterol levels are no longer in the red zone, his sleep apnea eased, and his energy returned.
He was also able to pick up an old hobby of his: running.
“Even when I’m traveling, I park my truck, put on my shoes, and go for a three- or four-mile run, something I wasn’t able to do before surgery.”
Advice for others
To those facing the same challenges he once did, Gonzalez offers some words of advice.
“The surgery helps you lose weight, especially in the first three months, but after that, being active is important,” he emphasizes. “If you’re not active, you might gain the weight back.”
The potential to gain weight post-surgery is why Scharf says education is such an important part of the surgery process.
“Anytime we talk about obesity, the most important thing for people to understand is that it is a chronic disease,” Scharf says. “That’s why we emphasize education for our patients, the community, and healthcare providers.”
Anyone suffering from obesity or other medical conditions related to obesity, such as type II diabetes, sleep apnea, high blood pressure, or high cholesterol, might be a candidate for sleeve gastrectomy or other bariatric surgeries. For more information, call us at 909-651-7091 or visit our website here.



