
Dr. Pillai, right, performs an endovascular treatment at Loma Linda University Health
Brain aneurysms are potentially life-threatening conditions that occur when a weakened section of an artery wall forms a balloon-like pouch. The wall of this pouch is thinner than the surrounding artery, making it vulnerable to breaking, which can result in a catastrophic bleeding stroke. If the aneurysm ruptures, it can cause severe bleeding and brain damage, often requiring immediate high-level medical intervention.
Traditional treatment for brain aneurysms often involves invasive procedures such as microsurgical clipping. In this approach, the surgeon makes an incision in the scalp, creates an opening in the skull, and places a metal clip at the base of the aneurysm to cut off the blood circulation to reduce the risk of rupture. While clipping is considered a safe and effective treatment for aneurysms, it is highly invasive and involves longer surgery times and extended recovery periods.
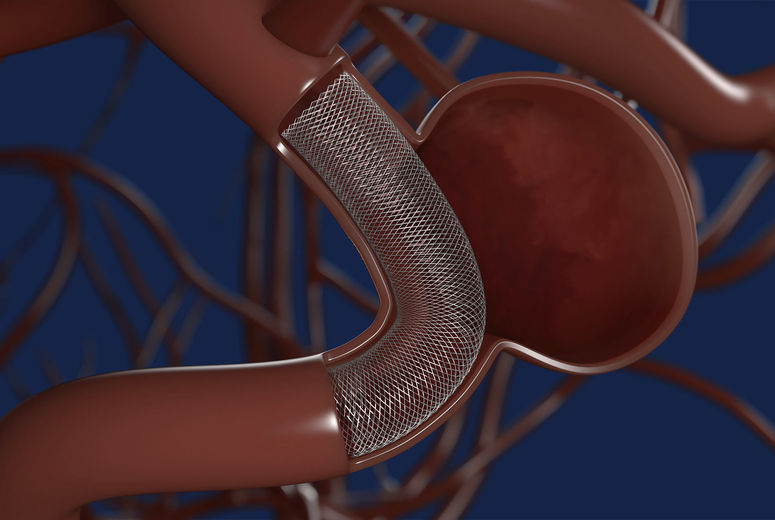
Promod Pillai, MBBS, MCh, FAANS, an endovascular neurosurgeon at Loma Linda University Health, highlights a less invasive option called endovascular treatment. This approach has gained significant traction over the past 30 years and is becoming increasingly popular for treating both ruptured and unruptured brain aneurysms in a minimal way.
What is endovascular treatment?
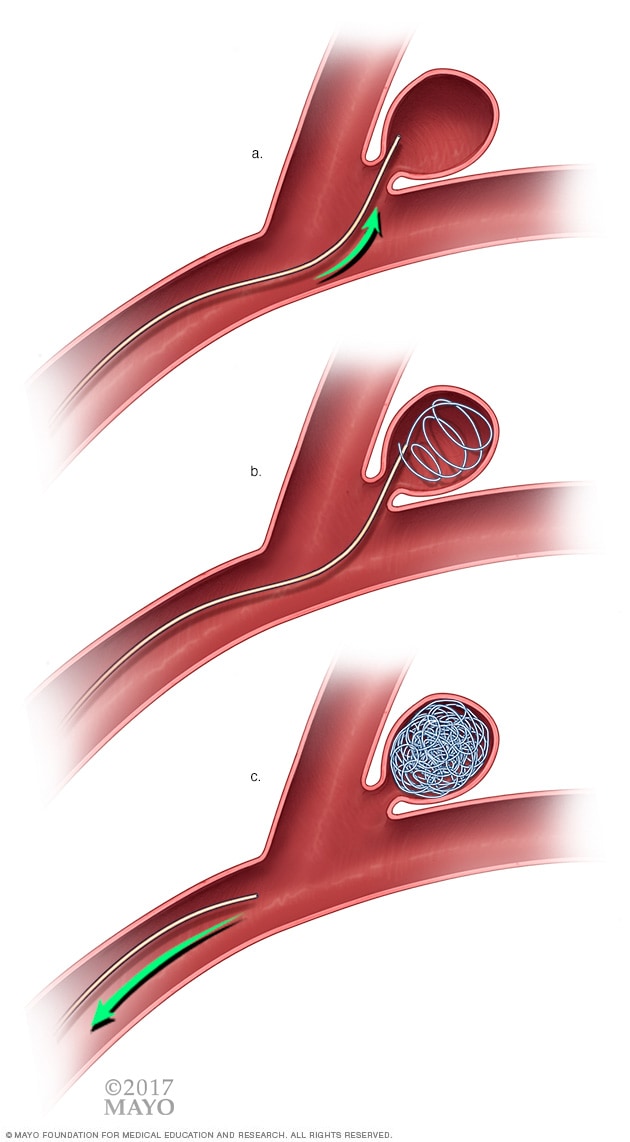
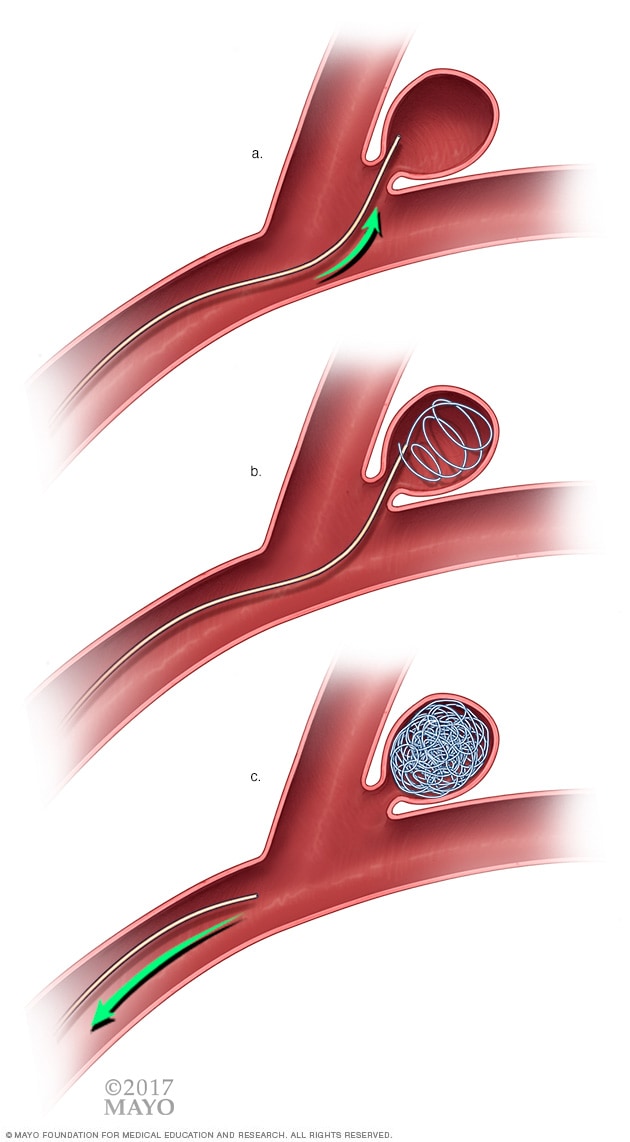
Pillai explains that an aneurysm is like a weak spot on a garden hose — while it's crucial for water to continue flowing through the hose, the weak area is at risk of bursting or disrupting the flow. Treating an aneurysm using the endovascular method involves “obliteration of the aneurysmal sac, working within the blood vessel, and preventing aneurysmal rupture, all while keeping blood circulation intact,” said Pillai.
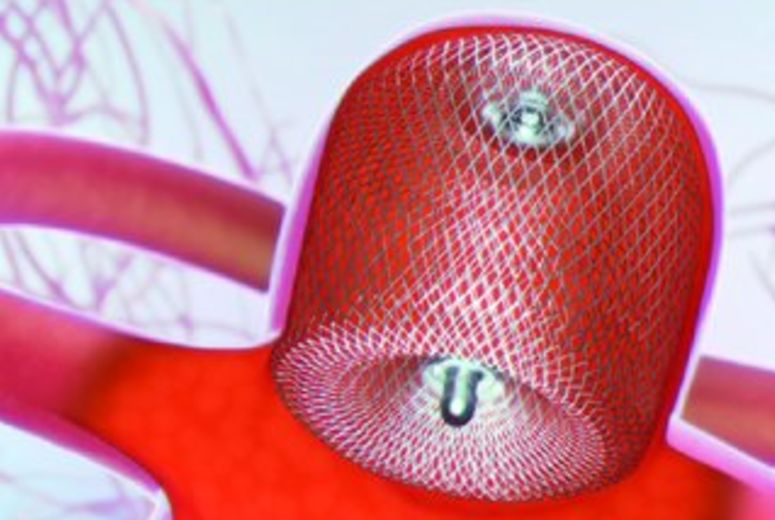
To do this, a microcatheter is inserted through an artery in the groin or arm and navigated through the vascular system to reach the targeted blood vessel in the brain. Once there, the aneurysm is treated from within the blood vessel using a technique called coiling, where thin platinum coils are inserted to block blood flow into the aneurysm. This allows the aneurysm to clot and keeps the normal circulation intact. Numerous studies have examined the effectiveness, safety, and risks related to coiling, including research from the American Heart Association Stroke Journal, which found that immediately after coiling, 90% of the aneurysms were adequately closed.
The benefits of endovascular treatment
Pillai highlights that the field of endovascular treatment has made significant advancements since the 1990s, including innovations like balloon-assisted coiling, stents, flow-diverting devices, and intrasaccular flow disruption devices. These techniques provide more precise and effective treatment options for aneurysms, particularly those located in hard-to-reach areas of the brain. Furthermore, endovascular treatment offers the following benefits:
Minimally invasive: Endovascular procedures do not require opening the skull or making large incisions, leading to shorter recovery times and less trauma for the patient. Most patients can leave the hospital within 24-48 hours after treatment. The minimally invasive nature of this treatment makes it a safer option for high-risk patients.
Less risk of injury: Since the procedure avoids directly manipulating brain tissue, the risk of causing additional trauma to the brain is significantly lower, making it a safer option for many patients.
Available for ruptured and unruptured aneurysms: Endovascular treatment can prevent aneurysms from rupturing and can also treat existing ruptures by preventing rebleeding, minimizing potential brain damage, and reducing the risk of recurrence.
Endovascular treatment vs. microsurgical clipping
When a person arrives at the hospital with a ruptured aneurysm, there is a short time span to decide which modality is the best approach. It’s crucial that each patient is transferred in a timely and safe manner to the appropriate high-volume center with multidisciplinary neurointensive care services, comprehensive stroke center capabilities, and experienced cerebrovascular surgeons/neuroendovascular interventionalists for the best outcome.
"Loma Linda University Health boasts one of the region’s top multidisciplinary teams, with specialists across neurovascular and endovascular surgery, interventional radiology, stroke neurology, as well as ICU and critical care physicians," said Pillai. "Treating an aneurysm requires a collaborative approach, and treatment decisions are made collectively to ensure the best outcome for each patient."
This multidisciplinary approach prioritizes patients and their medical needs for the best outcome possible.
While brain aneurysms can be life-threatening, endovascular treatment has made them far less of a death sentence than they once were. With the right care, brain aneurysms can be effectively managed, giving patients hope for a full recovery. For more information, call (909) 558-6388 or click here.