If caught early, NPH is the only treatable form of dementia
Early diagnosis of normal pressure hydrocephalus (NPH) is critical.
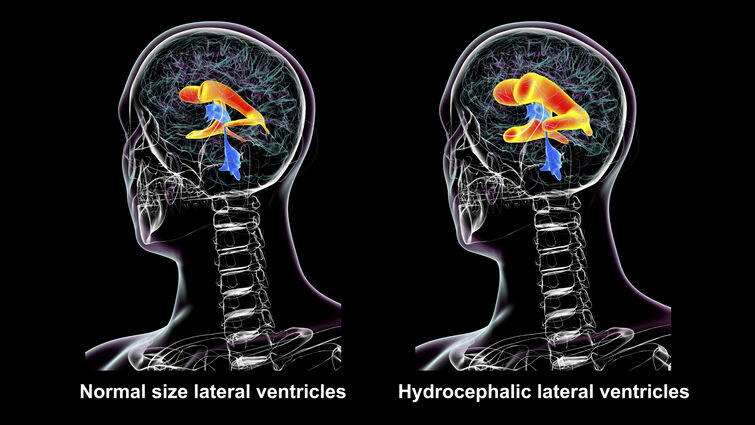
NPH is a condition caused by an abnormality in the flow and absorption of spinal fluid –– known as cerebrospinal fluid –– in the brain’s ventricles. This buildup of spinal fluid results in pressure on the brain that causes a characteristic triad of symptoms, including urinary incontinence and an unsteady gait.
If left untreated, NPH leads to more severe symptoms of progressive cognitive and memory decline that can ultimately lead to dementia.
Though the exact cause of NPH is not fully understood, when caught early, Warren Boling, MD, Chair of Neurosurgery, says it is the only treatable form of dementia.
“Unlike other types of dementia, where treatments may alleviate symptoms but cannot stop disease progression, NPH can often be prevented, reversed, or significantly improved with proper intervention through the surgical placement of a shunt to divert and drain a buildup of spinal fluid,” Boling says.
When the first signs of NPH become apparent –– urinary incontinence and gait disturbance –– the goal is to treat the condition before cognitive symptoms develop. NPH is very rare under the age of 60 but becomes increasingly common in older age groups.
How NPH develops
NPH results from the brain’s inability to properly absorb spinal fluid.
“Spinal fluid is produced in the center of the brain in fluid spaces called the ventricles by a structure called the choroid plexus,” Boling explains. “Spinal fluid circulates through the ventricle spaces over the brain’s surface and around the spine before being reabsorbed into the bloodstream.”
When the reabsorption process is impaired, it causes fluid to accumulate in the brain and the ventricles to enlarge. As the ventricles expand, they compress nearby brain tissue, disrupting brain signaling and causing the symptoms of NPH.
If left untreated, dementia can begin to develop over the course of a year or two.
NPH treatment
Though the exact reason for abnormal absorption is unknown, treatment focuses on diverting the spinal fluid away from the brain to another part of the body where it can be safely absorbed.
The most common treatment for NPH is the insertion of a ventriculoperitoneal shunt –– a small mechanical tube that reroutes excess spinal fluid from the brain to the abdomen, where it can be safely absorbed by the body.
During this minimally invasive surgery, a neurosurgeon places the shunt into one of the brain’s fluid-filled ventricles through a tiny opening in the skull. This tube connects to a programmable valve system that controls how much cerebrospinal fluid is drained. The entire system is placed beneath the skin, and the programmable valve allows physicians to fine-tune fluid drainage without additional surgery, reducing the risk of complications and improving long-term outcomes.
By redirecting the spinal fluid away from the brain, the pressure caused by fluid buildup is relieved, addressing and alleviating the symptoms of NPH. For most patients, this is a permanent solution.
However, like all devices, Boling says that shunts can fail over time.
“Shunt failure typically occurs when patients who initially experienced significant symptom relief notice a return of their symptoms,” Boling says. “When this happens, physicians must evaluate the shunt system and may need to replace or adjust it.”
However, once dementia is established, treatment can still provide benefits by relieving pressure, but it may not fully restore cognitive function.
Subdural fluid collection
One complication from shunting is the over-drainage of spinal fluid, which can lead to subdural fluid collections — fluid buildup outside the brain. This is why modern shunt systems use programmable valves, a revolutionary addition to NPH procedures that allow doctors to precisely control the amount of fluid being drained to prevent this complication.
Before the introduction of programable values, correcting subdural fluid collection required additional surgery –– often multiple surgeries –– to correct. Now, adjustments can be made quickly and non-invasively in a doctor’s office.
“The valve settings can be raised or lowered as needed to achieve the right balance of fluid drainage, which spares patients from additional surgeries and significantly improves long-term outcomes,” Boling said.
NPH is a serious but highly treatable condition, especially when caught early. With modern shunt technology and programmable valves, most patients can experience meaningful improvements in their symptoms and quality of life.
For more information, call 877-558-0800 or visit our website here.


