
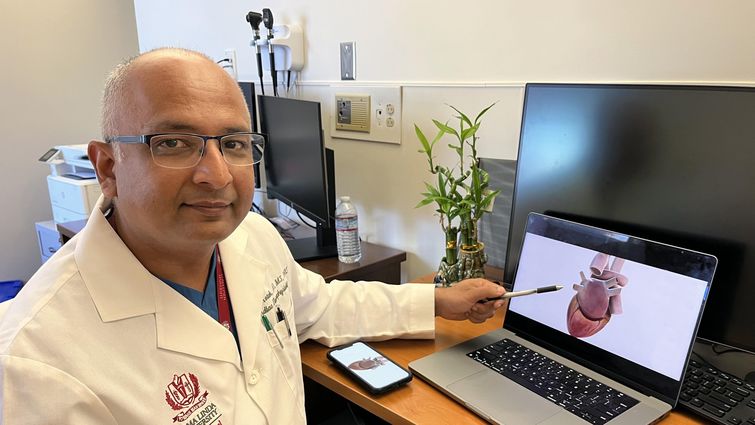
Kamal M. Kotak, MD, a cardiac electrophysiologist at Loma Linda University International Heart Institute, points to an interactive rendering of a human heart.
Receiving a diagnosis for atrial fibrillation, one of the most common types of irregular heart rhythms, often triggers a flurry of new questions or concerns from patients and loved ones, says Kamal M. Kotak, MD, a cardiac electrophysiologist at Loma Linda University International Heart Institute. For September’s Atrial Fibrillation Awareness Month, Kotak answers five commonly asked questions about treatment.
What is atrial fibrillation, and why does it require treatment?
Atrial fibrillation, or AFib, is a common heart rhythm disorder affecting more than 2 million U.S. adults. AFib can affect various people in different ways. Some people with AFib experience symptoms at varying intensities — heart palpitations, lightheadedness, dizziness, extreme fatigue, shortness of breath, chest pain — or no symptoms at all. Whether symptomatic or not, people with AFib face heightened risks of complications, especially stroke; AFib increases the risk of stroke by five times.
Read: Atrial fibrillation awareness: living with an abnormal heart rhythm
Treatment will depend on the patient’s profile and presence of other medical conditions, the type of AFib, such as whether it is paroxysmal versus persistent, how long it's been going on, and how it has affected the heart. Treatment is usually two-fold, with one part focusing on treating Afib itself to help with symptoms and the other focusing on stroke prevention (regardless of symptoms).
The generalized information about AFib treatments online may not necessarily apply to every individual, so seeing a heart rhythm specialist who can individualize treatment is critical. Every AFib case is different and gives treating physicians an opportunity to provide management options that are not only pertinent for the patient, but also sensitive to the patient’s and family’s needs and opinions.
Data show that the earlier patients and physicians initiate treatment of AFib, the better the outcomes.
What is ablation for AFib, and is it safe?
A large amount of scientific evidence tells us that ablation is superior to medical therapy in terms of long-term outcomes. Afib ablation is a minimally invasive medical procedure that treats abnormal heart rhythm. It does not involve any surgery or stitches. Patients are under general anesthesia for the procedure, during which physicians pass catheters and wires through a vein in the upper thigh to access the heart. Specialized software and tools create a live three-dimensional model of the patient’s heart so physicians can treat areas of abnormal electricity with millimeter-by-millimeter accuracy in real time.
The procedure typically lasts under two hours, and all the instrumentation is removed at the end. After a few hours of bed rest, patients can return home and resume their usual activities, except heavy lifting during the first week after the procedure.
The procedure is generally considered safe, with minimal risk of serious complications. The review of scientific data suggests that overall serious complications rate with AFib ablation procedures is less than 1%. Ablation relieves AFib symptoms, improves heart rhythm, and helps patients feel better overall.
How effective is ablation, and will AFib patients need more than one?
Ablation treats abnormal electricity in the heart's upper chambers (atrium). Though it depends on the nature of the AFib and patient profile, generally, 70-80% of patients experience significant resolution of their symptoms with minimal to no AFib.
Repeat ablations are uncommon but not rare. Over time, the heart can form new triggers, or old triggers become electrically reconnected, requiring another ablation procedure. Data show that ablation is superior to other treatment options for AFib in terms of efficacy, durability, and long-term outcomes.
What are blood thinners for, and why might they still be necessary after treatment like ablation?
AFib’s irregular and rapid heartbeat can cause blood to pool and stagnate in the heart’s upper chambers. This stagnant blood may form clots, which can break loose and travel through the bloodstream, potentially causing blockages in vital organs including the brain, and leading to severe complications such as stroke. Blood thinners prevent this blood clotting.
While treatments like ablation are highly effective in controlling AFib, patients may still experience AFib without being aware, such as during sleep, meaning there is still a risk of blood clotting and stroke.
Physicians use an assessment tool called CHA 2 DS 2 -VASc score to predict the risk of stroke in AFib patients. The score considers factors such as age, sex, history of congestive heart failure and stroke, hypertension, diabetes, and vascular disease. Results help the physician determine the need for a patient to take blood thinners to prevent stroke, regardless of outcomes from other treatments like ablation. In other words, stroke prevention is driven by patients’ risk profiles and not the severity of the Afib.
Are there alternative options to blood thinners?
Some patients may need to continue blood thinners but cannot because of major internal bleeding, significant bruising, poor balance, and a high risk of falls or other injuries. Patients experiencing issues with blood thinners, should talk to the doctor first rather than stopping the medications; stopping blood thinners is unsafe and can lead to stroke. In such cases, a minimally invasive procedure called left atrial appendage closure may allow patients to safely come off of blood thinner when indicated.
Read: LLUMC completes 200 minimally invasive surgeries to treat atrial fibrillation stroke risk
Loma Linda University International Heart Institute care teams are committed to providing patients with compassionate, comprehensive, and personalized cardiovascular care. To learn more, please visit lluh.org/heart-vascular or call 1-800-468-5432 to make an appointment.


