
Varicose veins, which are bulging, twisted veins visible under the surface of the skin, can occur in almost anyone, and they affect up to 35 percent of people in the U.S., according to the Society for Vascular Surgery. While they themselves do not cause severe medical problems, the presence of these uncomfortable veins could be an indicator of a greater health problem.
Ahmed M. Abou-Zamzam, MD, the division chief of vascular surgery at Loma Linda University Health, works with patients who suffer from vascular disease. Abou-Zamzam offers information to help understand the common vascular condition — varicose veins.
Valves and Veins
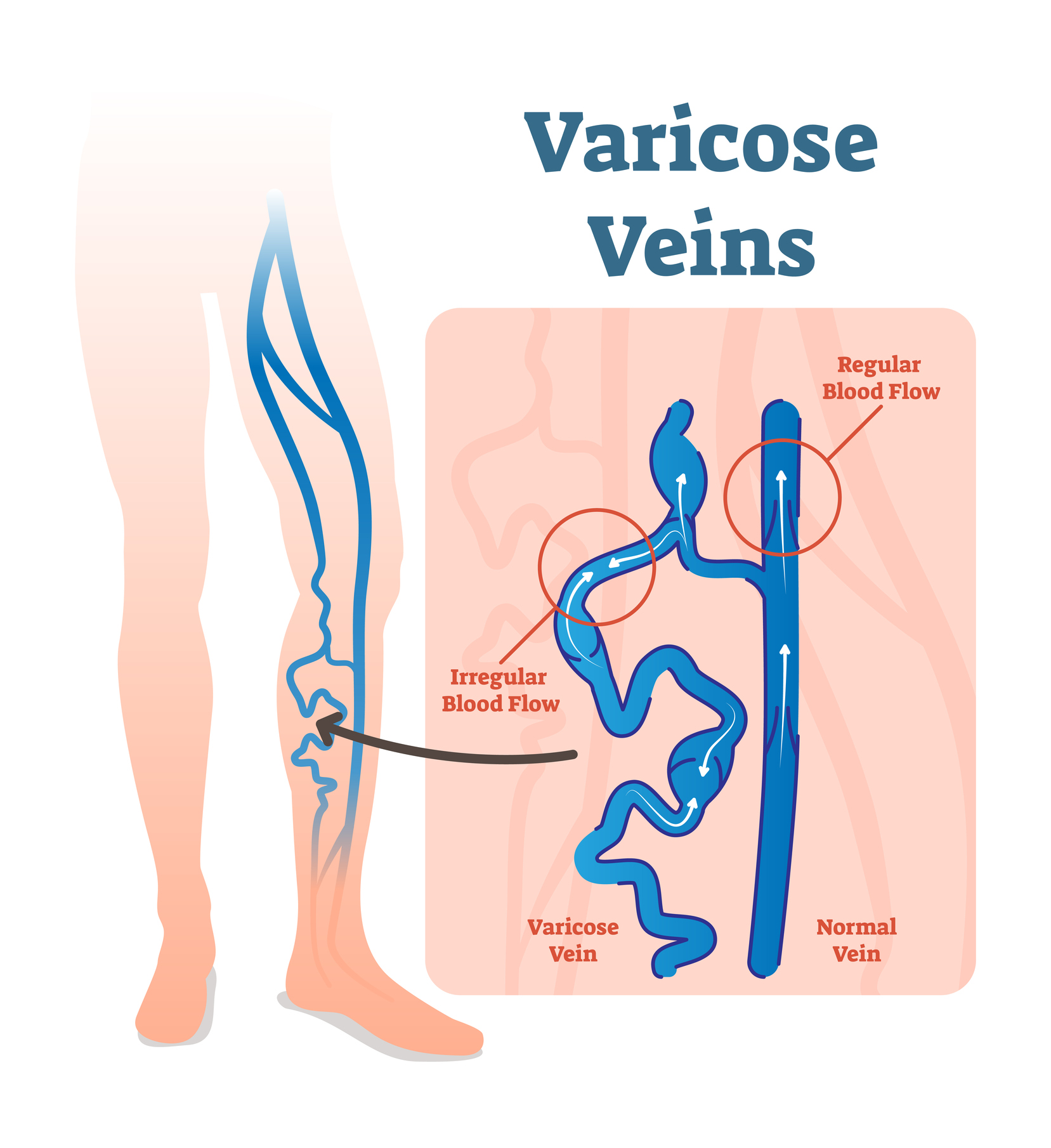
Veins are elastic blood vessels that carry the blood back to the heart after it’s carried to different parts of the body. In the veins, which are normally a low-pressure system, a series of valves — or one-way gates — open and close with ease, allowing the blood to travel from various body parts back to the heart. This opening and closing allows the blood to travel against gravity.
When those valves aren’t working normally, the blood can begin to go backward. “The valves don’t close quickly enough, or they don’t close completely, and this can cause the blood to back up,” Abou-Zamzam says.
That backward flow is considered venous insufficiency. When the valves become weakened or damaged, blood can collect in the veins. This causes the veins to become enlarged and spurs the formation of varicose veins.
Indicator of a bigger issue
Varicose veins are the most visible and well-known vein issue, but other manifestations of
venous disease — such as chronic leg swelling that worsens throughout the day, feelings of heaviness or pelvic pain — can be a sign of a venous insufficiency, Abou-Zamzam says.
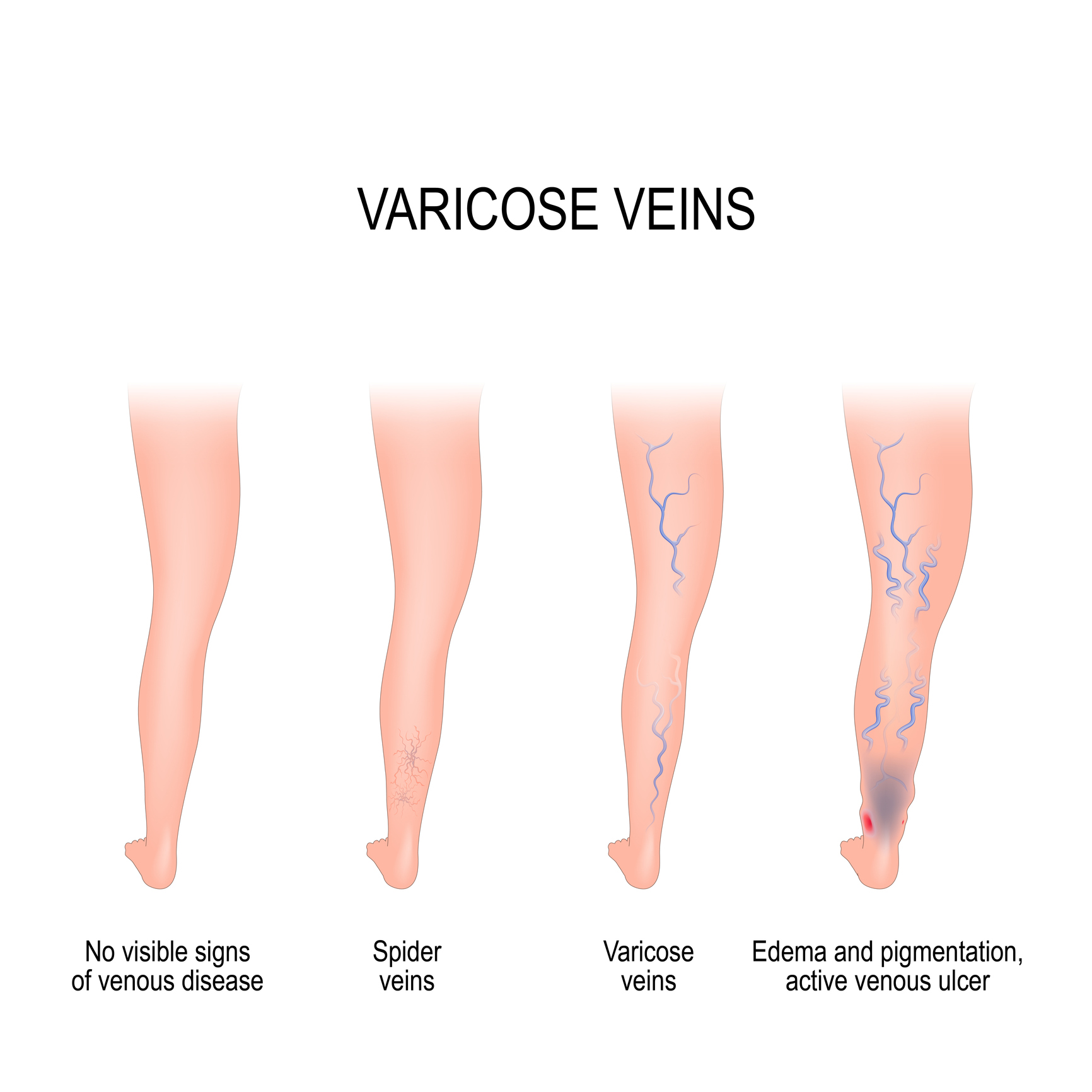
“The whole spectrum of the disease is called chronic venous insufficiency,” Abou-Zamzam says. That encompasses a spectrum of troubles with spider veins — little blue lines underneath the skin — or varicose veins, which are often bulging veins that get worse during the day, changes in the skin color or appearance, or the formation of ulcers.
“It’s a matter of degree,” Abou-Zamzam says. “With spider veins or varicose veins, if there are no additional leg symptoms, there isn’t any reason for concern because it’s unlikely that there is any danger.”
While varicose veins affect the veins close to the surface of the skin, with severe venous disease there is a chance of developing blood clots in the deep veins, which require immediate medical attention, Abou-Zamzam says.
In the absence of symptoms, many patients may still select options for treatment for cosmetic purposes. The Vascular Surgery Faculty at the Faculty Medical Offices has several minimally invasive procedures that can improve a person’s quality of life.
“We often look at management options in people who are otherwise healthy, but are chronically bothered by the presence of the veins,” Abou-Zamzam says. “They could benefit from the treatment, but if they have other multiple health problems, a procedure may not be in their best interest.”
When to talk to your doctor
If you have symptoms that may indicate a blood clot — such as pain, swelling or redness of the leg — Abou-Zamzam says it’s important to call your healthcare provider right away.
Without these more serious symptoms, there is still often reason to pursue treatment options. In the more severe aspects of venous disease, there is time missed from work due to leg discomfort, or eventual worsening that could lead to skin changes or ulcer formation. “There are many people who can benefit from treatment, which is often minimally invasive,” Abou-Zamzam says.
Most people need a simple ultrasound to document the presence of venous insufficiency and the location of their disease, Abou-Zamzam says. There are office-based procedures, such as injections, and some newer techniques — which include closing the large superficial veins altogether. These are performed as outpatient procedures, leading to quicker recovery.
“The strength of seeing a vascular surgeon is they have all available techniques at their disposal and will choose the most appropriate treatment for the individual, even if it is no treatment,” Abou-Zamzam says.
“If you see the vascular surgeon, they know how to treat all types of venous disease and can tell you whether a procedure is necessary,” he says. “I recommend being evaluated for venous disease if you have symptoms of chronic aching or swelling of the legs that becomes worse as the day goes on and it is relieved when the legs are elevated.”
Chronic venous insufficiency can be a nuisance and also holds the potential to decrease quality-of-life. “The way I look at it, a little bit of discomfort every day adds up through the years to a lot discomfort,” Abou-Zamzam says.
To learn more about venous disease or to schedule an appointment or consultation with one of our vascular experts, call 877-558-6248.
