The TAVR procedure is a non-invasive alternative to open heart surgery for aortic stenosis
Before undergoing a life-saving aortic valve replacement, Rickey Rodriguez couldn’t walk from one room to another without becoming winded and needing to sit down. Unaware that his aortic valve had developed severe stenosis — a condition that narrows blood flow to the heart — Rodriguez was hospitalized and in need of a new valve.
Due to other health complications, including concurrent lung disease, Rodriguez was not a suitable candidate for open-heart surgery, the traditional treatment for aortic stenosis. Instead, doctors recommended he undergo a Transcatheter Aortic Valve Replacement (TAVR) –– a minimally invasive procedure designed to replace a failing aortic valve without the need for open-heart surgery.
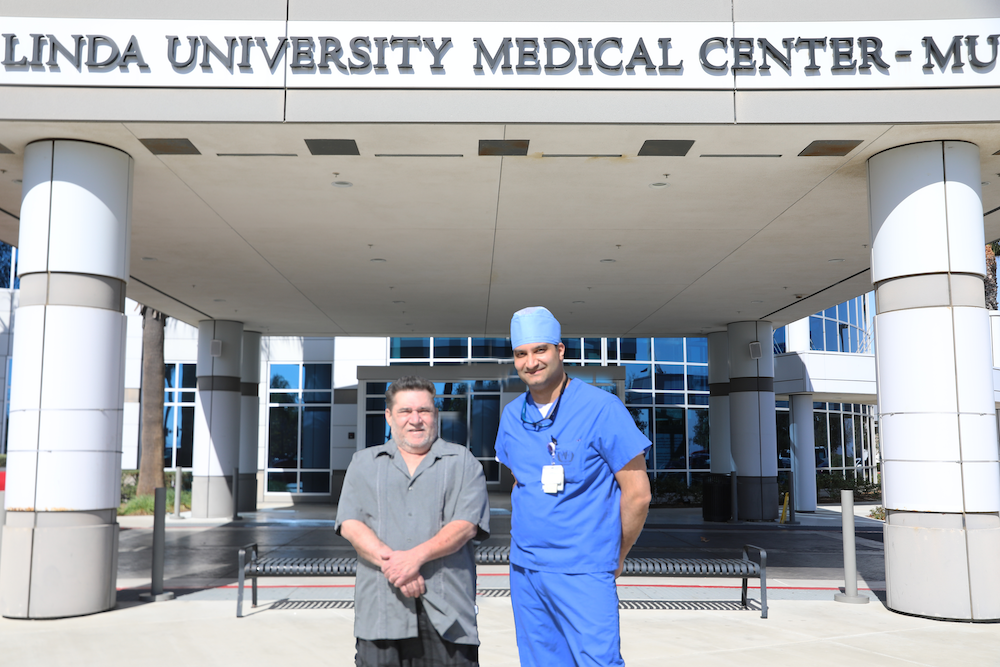
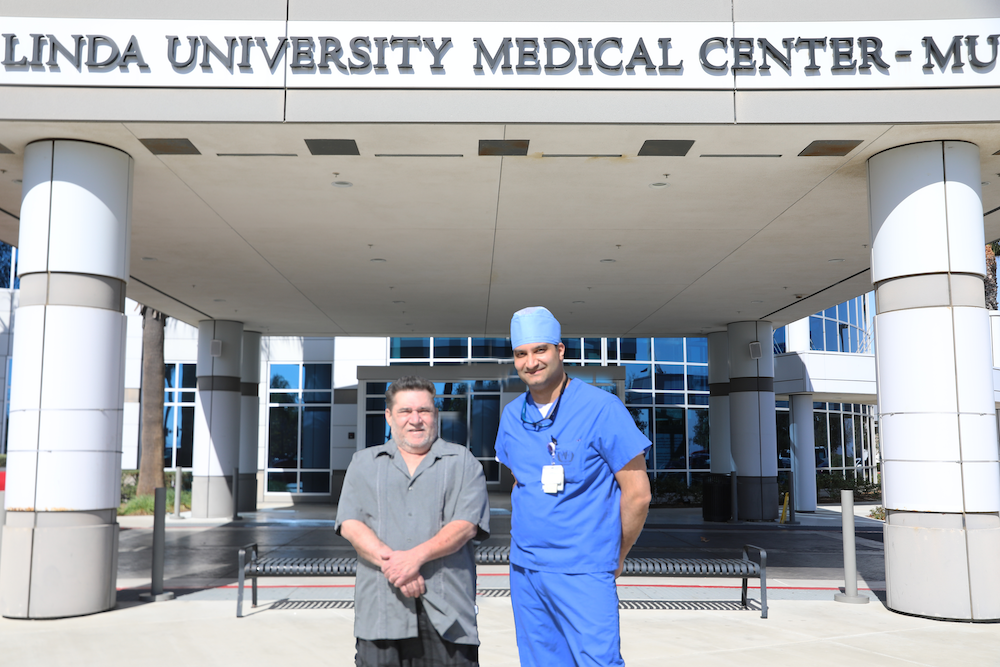
Within a week of his 2024 hospitalization, Niraj Parekh, MD, a cardiologist at Loma Linda University Medical Center – Murietta, and the multidisciplinary team in the catheterization lab successfully replaced Rodriguez’s valve, effectively saving his life.
However, this wasn’t the first time Rodriguez had faced a serious health battle. For over 10 years, he struggled with various medical problems so severely that in 2014 he was forced into early retirement, which left him dependent on oxygen tanks to breathe.
“When I started to have problems, I would get really dizzy and blackout,” Rodriguez said of his symptoms. “But I was the kind of guy who didn’t want to go to the hospital.”
In addition to oxygen tanks, Rodriguez relied heavily on over-the-counter medications to help his breathing issues, which he believed were caused by mucus buildup. But in 2022, after suffering for three nights with mild heartburn symptoms that grew more severe each day, Rodriguez went to the hospital and learned he was having a heart attack.
Using advanced cardiology techniques, Parekh and his team identified significant blockages in Rodriguez’s arteries and placed seven stents to restore blood flow and stabilize his condition.
Although treatment for his heart attack initially improved his quality of life, Rodriguez was hospitalized again in 2024 with shortness of breath and dizziness. To determine whether his symptoms were related to worsening lung or heart disease, doctors performed an echocardiogram, which revealed a severely diseased aortic valve.
“We did a full workup on his aortic valve, and given his lung issues and other comorbidities, he wasn’t a great candidate for open-heart surgery,” said Parekh. “Multiple surgeons agreed that a TAVR option would be better.”
After stabilizing his condition by managing his fluid levels, Rodriguez was ready for the TAVR procedure within a week of his initial hospitalization — one of the fastest turnarounds in the country compared to the national average of 90 days.
Unlike open-heart surgery, which requires a large incision in the chest and splitting the breastbone to access the heart, a TAVR delivers a bioprosthetic valve, typically made from pig tissue, through a catheter inserted into the femoral artery. The heart is temporarily paced at 180 beats per minute to ensure stability while the valve is precisely positioned and deployed. Furthermore, unlike open-heart surgery, which requires weeks of recovery, TAVR patients typically go home within 24 hours.
For Rodriguez, the entire TAVR experience was the answer to years of sickness and suffering.
“They prayed for me before the procedure, which meant a lot,” Rodriguez said of the kindness he received from the entire staff. “The whole experience was smooth, and I felt no pain at all.”
Within a day of the procedure, Rodriguez was home, recovering, and breathing without oxygen support for the first time in years, something he thought he’d never experience again. As for the success of the procedure, Parekh emphasizes that each TAVR is a direct result of a highly coordinated effort.
“We have a strong, collaborative team — surgeons, nurse practitioners, coordinators, interventionalists, and anesthesiologists — who are dedicated to taking on any challenge and figuring out the best way to care for each patient,” he says. “We assess how sick patients are and work to optimize their condition so we can get them treated as soon as possible.”
For Rodriguez, this high-quality care and team effort have allowed him to experience dramatic improvements so that he can finally start enjoying his retirement.
“They saved my life twice now,” he said. “I never knew there were such good, decent, nice people in the world.”
For those struggling with similar symptoms, Rodriguez’s message is clear: don’t wait. Seeking help could be the difference between life and death. For information on maintaining a healthy heart or heart procedures, visit our website here.


