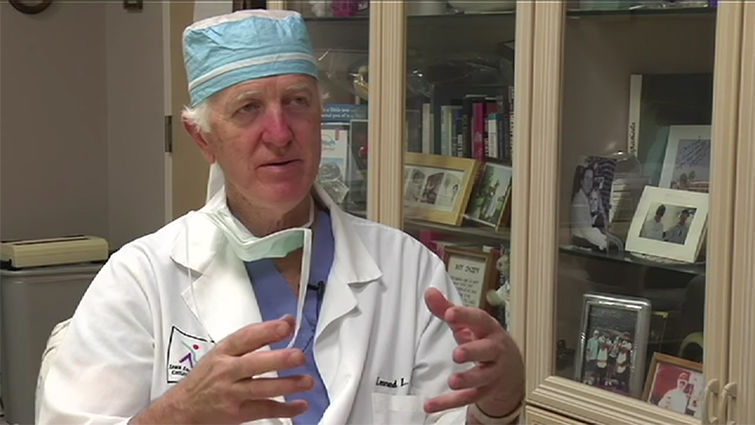
Surgeon Leonard Bailey shares the stories of Baby Fae and Baby Moses.
It was my privilege to sit down [in 2007] with Leonard L. Bailey, MD, and listen as he recounted his experiences leading up to Baby Fae's historic heart transplant on October 26, 1984—just 12 days after her premature birth with hypoplastic left heart syndrome. The heroic efforts of Bailey and his team to save Baby Fae included the use of a baby baboon heart. Her brief life gripped the world as few stories have and raised awareness of the need for recovery of infant hearts and other organs to give these otherwise healthy children a chance to live and thrive. Bailey has a deep appreciation for the laboratory animals who gave the gift of life so that transplant research could take place. – LK
While I was still in training, I had already made up my mind that someone needed to investigate transplantation in newborns. At that time, babies born with certain kinds of exotic heart disease weren't even treated—they were set aside to die. And they uniformly did that.
I had encountered some of those babies. We tried various things to see if we could prolong their lives. Mostly we prolonged their dying, maybe by a few days. But we had no success at all in saving them.
I'd had a fascination with transplantation since visiting a laboratory at Stanford while I was in medical school. I thought the natural thing would be to put the two together—babies born with incurable heart disease who are dying, and this transplantation technology that hadn't found life yet in this age group.
Oddly enough, one of the very first transplants—and probably the first transplant done in this country human to human—was on a newborn baby. Dr. Adrian Kantrowitz in New York had done a few infant animal tranplantations in his laboratory, and had this same notion that transplantation ought to be good for babies with broken hearts too.
So he made that attempt in 1967. The baby actually didn't survive. I believe they were able to get the baby out of the operating room and into the intensive care unit for about five or six hours, and that was as far as it got.
Of course, transplantation of the heart was all the news at that time. Dr. Chris Barnard in South Africa had done the first human heart transplant using another human heart.
Dr. Jim Hardy had put a chimpanzee heart in a human down at the University of Mississippi, in Jackson, in the mid 1960s. He had a patient with terrible heart disease whom he couldn't wean off the heart/lung machine. He'd always had an interest in the idea of transplantation but hadn't worked it out fully. Nevertheless, he went down to the lab and found an aging chimpanzee, harvested the heart, and put it in this fellow. It worked for awhile, but it wouldn't sustain his circulation beyond the operating room.
When they performed an autopsy on the chimpanzee's heart, lo and behold, the old chimp was suffering from severe coronary artery disease. It probably wasn't really a fair situation.
That wasn't something done in isolation. Dr. Keith Reemtsma had transplanted chimpanzee kidneys into human beings at Tulane in those early days, and actually had done reasonably well with that group of patients. One ended up surviving eight or nine months and was back on the street living a reasonable life. That's at a time, to put it in perspective, when we really didn't know anything about transplantation or about how to suppress the immune system. We had some arcane medications to use, but nothing very good yet had come along.
When I returned to Loma Linda from training, the surgery department was very generous with me. They budgeted some money for a laboratory. We got the laboratory going again—it had kind of fallen idle for a while. Dr. Lou Smith, who did the first organ transplant at Loma Linda University, had an active laboratory program going for a number of years. He had become so busy clinically that he couldn't keep it going, and it had fallen quite idle. I didn't see any merit in that.
So we found some funding, put the lab back together, and hired some technical people to help with transplanting and looking after some little newborn goats. We chose goats as recipients because, for one thing, they're lovely little animals, easy to test, and smarter than most animals—and very hardy, as opposed to lambs, which aren't nearly as tough. So lambs, at some level, became donors, and goats were always the recipients. And they were available; we had a farm facility where we raised them.
We would take a baby goat a few days old and do a heart transplant-orthotopic heart transplant—and that little baby would be jumping around the cage that evening. The next day, we would put it in the pens with other goats, and then in a week it would be back out on the farm with its transplanted heart. What we wanted to learn was how far they would go.
One of the greatest stimuli I had when I was studying pediatric heart surgery up in Canada was the awareness that the newborn immune system is indeed fairly special—it has very little of the aggressiveness of the older child or an adult. It has no experience, which helps. And much of the suppressor type behavior is still intact in the newborn.
So the possibility that a newborn could receive a graft and actually grow up without any immune suppression was curious enough. We were able to demonstrate close to that. We had a baby goat named Livingston who was transplanted as a newborn and grew to 6 months of age with no immunosuppression at all.
On average however, the transplanted goats without immunosuppression survived about two and a half months. Then they began a slow rejection process. So their immune systems, we knew from that experience, were intact—they were just much more accommodating as newborns.
Then we wanted to know what we could do to manipulate the immune system some way or other. We set up a series of experiments with various modifications to observe the host immune response. As it turned out, none of the modifications lengthened the mean survival rate.
A fellow by the name of John Borel, in Basil, Switzerland, was working for a pharmaceutical house. He had found a fungus-like substance out in the hills. His job was to study it and see if there was anything there that he could make a medicine out of. I think he was originally looking to see if he could find something that would be effective with allergies.
But he began to study the immune properties of this substance and how it might alter the immune response in a host. It was pretty promising—something called cyclosporin. It was called cyclosporin-A at that time. I suppose they thought there would be cyclosporin-B, -C, and -D.
So this substance was being studied in the laboratories of the Swiss pharmaceutical house and by other laboratory investigators around the world. Here in the West, Stanford had access to it. I contacted John Borel—I'd met him earlier at a presentation I was making one time down in Texas. He had agreed to send me some of this material.
He began to send this material to me in brown jars. It was a powder. You had to mix it with some oily substance in order to get it suspended. And then you could begin to quantitate how much you were giving an animal. We prepared a group of little goats for allograft transplants—goat to goat. Mind you, there were frequently different subspecies of goats, but they were similar enough.
We performed the transplants and treated them with cyclosporin all along. With that, they lived indefinitely. That was all it took. Cyclosporin-A became the mainstay of our immunosuppression.
That took our breath away—the fact that we could transplant a baby at birth and have that baby grow up with nothing more than receiving injections of this oily substance. The baby goats would go down to the farm, grow up, become big herd animals, and actually grow old. And if they didn't get in trouble, they would die just of old age.
As goats do sometimes, they get into a lot of trouble with things they eat. One of our older goats, one named Sigmund, was about 3 or 4 years old, and he got into our rubber glove supply—he ate all of these rubber gloves and died of an intestinal obstruction.
Then we thought, "Well, how are we ever going to transplant baby humans? We don't have a system for identifying potential donors for baby humans; if we're going to transplant them, we're probably going to have to start with cross-species." So we began to transplant lamb hearts into goats, and even pig hearts into goats. We had some really fascinating survival with these cross-species transplants, using cyclosporin-A alone.
And then we began to study what would be a potential donor for a human being. Chimps were out, and orangutans and gorillas—they're all endangered. We wouldn't think of using an animal like that. But baboons seem to have a life of their own; they're extraordinarily plentiful. There are actually programs to control the populations in South Africa and places like that. They are hardy animals and reproduce easily.
We thought, "Now here's a subject we can study." We soon discovered that more than 80 percent of the DNA in a baboon is identical to that of a human being. The human leukocyte antigen (HLA) typing method is used to identify your tissue as being you and not your neighbor. We found we could actually type baboons. And we could put baboon cells and human cells together and pretend to do transplants in the laboratory, and find out which baboon might be the most compatible with any one human being's sample.
There were three or four important immunologic bench studies that we could do to select a baboon donor. The first thing we did was acquire some baboons. We contacted our friends in southwestern Texas at a huge primate center—probably one of the best, if not the best one, on the planet. We told them what we wanted. We preferred juvenile female baboons. We didn't want to have any male baboons growing up and tearing up the cages.
Sure enough, they were able to provide some juvenile female baboons. They would wean the baboons there and then ship them out to us. So we had about a dozen of these juveniles that we called our donor panel. We did some other bench studies—for instance isolating a baboon heart and then perfusing that heart with human blood in an isolated heart preparation—and did the same thing with the goat and pig hearts. With the barnyard animals, none of the hearts functioned at all; the little baboon heart functioned beautifully for 12 hours in that experiment.
We needed Institutional Review Board approval. It took 14 months from the time we started to when we received approval from the board. As I recall, Dr. Dick Sheldon was the chairman of the board at that time. He was a terrific ally—not that he was all for it, but he just did a really superb, objective job of assessing and moving his board through the process.
We had to bring in external reviewers. We brought in a number of people to review the protocol and give us their opinions. These were prominent transplant people who were involved in the process, and we had various opinions of course—some were somewhat supportive, some were not supportive at all.
One of the opinions was, 'Why not?" That opinion came from Dr. Sandra Nehlsen-Cannarella. And she agreed to serve as our chief corresponding immunologist as we went forward. She told us she would be available—if we ever tried this clinically, she would be on the next plane and come out and help us. And sure enough, that happened. Ultimately, Dr. Bruce Branson hired her and she moved from where she was in New York out here, and was here for a number of years as the chief of immunology.
The time came when we were very close to being ready to start. The protocol was to do five of these cross-species transplants with newborns with hypoplastic left heart syndrome. I was stopped in the hall one day and one of our pediatric cardiologists, Dr. Gene Petry, asked, "You know, Bailey, how's that protocol coming? I happen to have a baby in the nursery now with this problem. Are you interested?" I said, "Well, let me do some checking." I got back to him and said, "Yes, I think we are." He said, "Well, I've discharged the baby home to die. The baby and her family live up in the high desert. I'll have someone contact them and see if they have any interest."
So one of four neonatologists, Dr. Doug Deming, called this mother and said, "We have this protocol that's never been tried just like this before. Do you have any interest?" And they thought about it and phoned back, and said they thought that they might have an interest and that they'd like to talk more about it. We invited them to come down—we spent hours actually in discussion. Part of the protocol meant that they had to sign a form saying they were interested. And then at some point or other, within another 24 hours they had to sign again, saying they were still interested and would give us the consent to go forward.
After the first meeting, they indicated they wanted to go forward with it. The baby was up in the desert and beginning to die. They brought the baby back down. We did what we needed to do, which, in those days, wasn't very good, to try to keep the baby alive. The assays comparing the baby with the baboon panel were supposed to have taken about a week, but on or about the sixth day or so of this effort, the baby was clearly going to die that day. We needed to move forward so Dr. Nehlsen-Cannarella read the tests a bit early. As it turned out, the tests identified one of the baboons that was most compatible, and that little baboon was set up to become the donor.
I should mention that, months before, we had screened these juvenile baboons for infectious disease—for everything from A to Z that we knew and were able to test for in those days—and we knew they were clean. They had come to us clean, but we retested them to be sure they were to our satisfaction.
Now we had this donor panel that was ready to go. It came down to the day. I knew that Baby Fae was getting closer and closer to dying, and so we knew that we were going to do it the next morning. We heard rumors toward the end of our preparation that some newspaper up in the desert had heard about it. I don't know how the leak happened, but it did. We were able to placate the news people at least until after the transplant was done. Fortunately, the pre-operative story stayed local and didn't spread.
We had done many of these newborn transplants in the laboratory; transplanting with a human newborn was just the next natural thing to do. I don't recall being terribly nervous about it; I didn't have much angst over it at all. Actually I was at a restaurant in Redlands the night before with my wife, Nancy. We discussed the situation together a little bit—what the consequences might be.
We didn't have any idea of course what might happen, but we thought we should at least discuss it, and we did.
The next morning, I popped up and was down at the lab by about 6:00 in the morning. Howard Shattuck, our surgical assistant originally brought in from Johns Hopkins, was my right arm in the laboratory surgically, helping me with the transplants. So I had him on the other side of the table with me, as well as some residents.
We gathered around the operating table. I brought the heart up from the lab. I remember taking the heart out and going up the back stairs and into the operating room. We had Baby Fae all ready. I arrived with the heart, we made the incision, and went to work. We'd done it so many times, although we'd never really worked with hypoplastic left heart syndrome. It cast a slightly different nuance on the surgery, because the whole aortic arch had to be reconstructed as part of the process. We had dreamt of how it might go, but we'd never actually done it in exactly this way in a baby.
We were blessed. It just turned out beautifully. Her response to the surgery was just perfect.
I expected some reaction to it. I remember what went on with Dr. Chris Barnard, for instance. It was like a three-ring circus in Capetown.
I didn't think that Baby Fae's transplant would set off so many alarms. I thought there might be some regional interest, but the story became world news. That part of it was a little surprising. And it was a bit of a distraction—it did affect her care. We felt like we were operating in a glass bowl.
Initially, Dr. Branson and others took over talking with the news people. Dr. Nehlsen-Cannarella and I, and our team were focused on Baby Fae. We were there day and night. We didn't know exactly what to expect, and didn't want to miss anything either, and so we were just there. And then of course, toward the end, it became heartbreaking—we were losing her and we didn't quite understand why. Her heart was "gangbusters" still, and yet she was dying. We knew we hadn't overdone the immunosuppression or anything like that.
To this day, it's a bit of a mystery what went on. Anyhow, she died, and that was heartbreaking. We invested a lot of time, energy, and effort. We had gotten to know her family.
It was also an institutional thing. I don't recall the institution ever being quite as unified on anything as over this little baby. We all wanted her to go further, and it was a major letdown.
And then, of course, there were all sorts of second guessing, "seventh inning" discussions, that went on, some of which we tried to listen to with an objective ear and learn from. Some were just wild—show business, I guess you'd say.
The media frenzy finally boiled down to a simmer. It was an election year, and you hardly knew Ronald Reagan was being re-elected. This process was right at the same time. It nearly knocked him off the front page!
The hate mail and threats poured in for a long time, so much so that the Redlands police wanted us to let them open our mail and things like that. They were excellent. They were a great hometown police department. They just took over. Wonderful. We felt very secure. We had two little children, Connor and Brooks, who were quite impressed when the police came up to the house and gave us all lessons about how to take care of ourselves.
When we did the first allograft transplant a year later with Baby Moses (his real name was Eddie), wouldn't you know there were several busloads of people who came out to picket the house. The Redlands police, stars that they are, only permitted these people to demonstrate in front of our neighbors' house—I don't think our neighbors were even home. Up on our property and in our house, there were officials from the police department guarding us.
Just like Baby Fae, this first allograft transplant with Baby Moses was very serendipitous. It just so happened that Eddie was still in our hospital. An obstetrician from the Bay Area called me and said, "I know what you did for Baby Fae. Are you still doing transplants, because I have a baby here with birth asphyxia, and the parents want the baby's organs donated. Nobody else wants baby organs except you." I said, "Well, I think we do want that heart."
We talked to Eddie's mom and dad. They wanted to move forward. They'd lost a baby the year before to heart disease. So we brought that donor baby down to Loma Linda and we performed what it turns out was the first successful clinical newborn heart transplant, done a year after Baby Fae. That hit the news too and went all around. I think initially the story received a life because people thought the heart was from another baboon donor. But then it took on a life of its own because he stayed alive. And for the next several months there was intense interest.
More important than the news—though that was vital—was the development of a donor base. Procurement agencies said, "Well, if Bailey's really going to do this, we'd better get ourselves up to speed too." So procurement agencies all around the country began to make something out of this human story that was out there. And people began to consider donating if their baby had birth trauma or brain death—they began to consider organ donation.
Procurement agencies also began to work in that direction. So, ever since Baby Fae and Baby Moses, there has been a fairly steady flow of organ donors. There aren't that many—it's not terribly practical—but there has been a steady flow of somewhere around 100 a year nationwide.
One comment that I would make is that Loma Linda as an organization enabled it and embraced it, and we pulled it off as an organization better, I think, than had I been at any other academic center in the world. With Baby Moses, we crossed the barrier of transplanting a newborn, something which hadn't been accomplished previously.
In 1984, the same year we transplanted Baby Fae, Sir Magdi Yacoub in London had performed an allograft on a newborn, and came close to being successful, but the baby died. To me, Loma Linda's claim to fame is the fact that our baby, Eddie, is still living. He was off in a corner dying when we found him. We brought a heart down from the Bay Area and put it in. Eddie is living up in Las Vegas and working at one of the hotels there. He [was] 21 years old [in 2007].*
So that's how it all comes around. The rest, as they say, is history.
Source: Scope, Spring 2007
To view the full-length documentary, visit "Stephanie's Heart."
*Eddie (Baby Moses) still lives in Las Vegas. Every so often, he comes to Loma Linda University Health to visit his friends—especially Bailey. He was born November 20, 1985, and will turn 31 years old in November 2016. He is the longest living infant heart transplant recipient in the world. To date, the longest living heart transplant recipient in the world (according to the 2013 Guiness World Records book), John McCafferty, passed away at the age of 73 on February 9, 2016—33 years following his transplant surgery at 39 years of age (source: BBC News story).
