
Men who have undergone a prostate-specific antigen test (PSA) that resulted in a high PSA number may have questions: “What could an elevated PSA indicate?” and, “What can I do next for my health?”
Herbert Ruckle, MD, FACS, chair of Loma Linda University Health’s Urology Department, answers your top questions about receiving and interpreting an elevated PSA result and what to expect thereafter. “It is important for men to know their PSA number and understand what it means, so they can engage in shared decision making with their doctor and decide what is best for their care moving forward,” he says.
What is PSA, and how do PSA tests work?

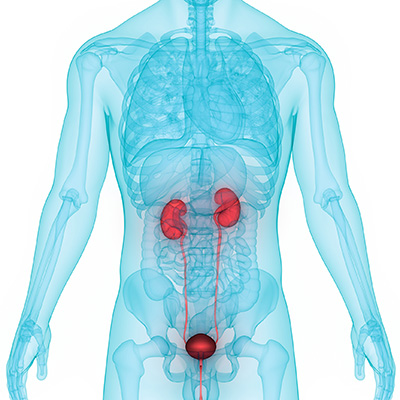
The prostate is a small, apricot sized gland that sits below the bladder in males and uniquely produces prostate-specific antigen, a protein that circulates in the bloodstream. A PSA test is a blood test that measures prostate activity, reporting results as nanograms of PSA per milliliter of blood (ng/mL). Prostate cancer screening is generally recommended for men 55-70 years old or as young as 40 years old for men with a family or racial history that places them in a high-risk group. To benefit from prostate cancer screening, a man should be generally be healthy enough to have a 10-year life expectancy.
The range generally accepted as a “normal” PSA level spans from zero to four nanograms of PSA per milliliter of blood, though there are exceptions based on age, race, and risk factors. You and your physician can discuss whether any such nuanced situations apply to you. Keep in mind although a PSA test can certainly detect high levels of PSA in the blood, it is not enough to diagnose a cancer because an elevated PSA is not a definitive sign of prostate cancer.
My PSA is elevated — what could it mean?
First, realize that having an elevated PSA does not necessarily mean you have cancer in your prostate. Other causes for an elevated PSA include:
- infection, instrumentation of the urinary tract, disruption, trauma, or manipulation of the prostate
- certain conditions like prostatitis or enlarged prostate
You and your doctor will work together to identify any of these possible contributing factors to your higher PSA through measures like checking for urine infection, reviewing for history of instrumentation, inflammation and discussing family health history. You and your doctor may identify such a cause, address it with treatment, and re-test PSA to see whether the level has appropriately decreased.
If you and your doctor do not rule out any other causes, you will likely need to undergo another PSA test and a digital rectal exam. During this exam, a physician inserts a lubricated, gloved finger into the rectum to reach the prostate and feel for any lumps or hard areas. Continued abnormal results from the PSA test or rectal exam call for further investigation to identify clinically significant prostate cancer.
What secondary tests are available to me?
Various secondary testing methods are at your disposal should you need more information before engaging in shared decision-making with your physician about further prostate cancer screening. It could also be helpful if your PSA test or rectal exam results place you in a "gray area" of risk for prostate cancer.
- PSA free-to-total-ratio, or prostate health index (PHI): can help improve the accuracy of the standard PSA test by discerning whether your risk of having prostate cancer is as low as 10% or as high as 50%.
- PSA velocity: If you've had previous PSA tests, your physician will look at them to determine how quickly your PSA levels have changed over time. A steep PSA level increase over a short period (an increase of higher than 0.7 nanograms of PSA per milliliter of blood per year) often correlates with a prostate cancer diagnosis, Ruckle says.
- Urine tests: One of which detects PCA3, a noncoding RNA gene that is only in your prostate. Too many copies of PCA3 in the urine indicate a greater chance of having prostate cancer.
- MRI of the prostate to image for biopsy targets.
Based on any of these results, the doctor will recommend a prostate biopsy if they suspect cancer.
What does an ultrasound-guided prostate biopsy involve?
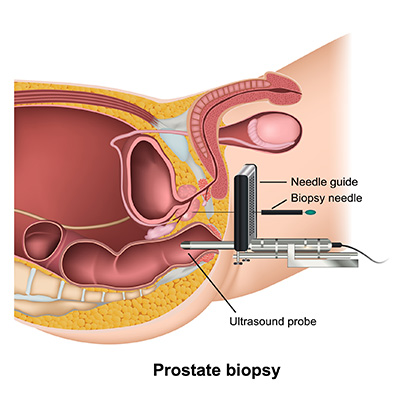
During an ultrasound-guided prostate biopsy, physicians insert a thin, flexible tube with a tiny camera into the rectum to reach the prostate. They then carefully guide a very small, hollow needle into the prostate to take some samples of the organ’s tissue. Next, a pathologist examines the collected tissue under a microscope to search for any cancerous cells.
Before starting the procedure, physicians will ensure you do not have an infection and do not take blood thinners. The procedure takes only around 10 minutes, during which the patient has local anesthesia. Ruckle says the chance to find a curable prostate cancer and have the opportunity to prevent it from harming you far outweighs the transient, mild discomfort and risks of the biopsy experience.
What if my biopsy results are negative?
A negative biopsy does not definitively exclude the presence of cancer. After a negative result, you will have a PSA test every three to six months. If the PSA remains elevated, the physician will recommend a second biopsy.
The closer you follow the patients with negative biopsies, the less likely you are to miss a clinically significant cancer.Dr. Herb Ruckle
For a second biopsy, MRI imaging is typically performed. An MRI-guided prostate biopsy uses advanced, more accurate imaging to take a biopsy and detect a cancer missed in the first ultrasound-guided biopsy. If this second biopsy comes back as negative, the physician will continue to keep a close eye on your PSA levels with the variety of tests, and you may need to undergo additional biopsies. “The closer you follow the patients with negative biopsies, the less likely you are to miss a clinically significant cancer,” Ruckle says.
What if my biopsy results are positive?
Following a positive biopsy result, the next step is to determine the cancer’s staging — the extent to which cancer has developed by growing and possibly spreading. You will undergo a bone scan, an MRI of the pelvis, or a CT scan. In the near future, PET scanning specifically for prostate cancer will be widely available. Ruckle says you and your physician should customize your prostate cancer care based on your desires, fears, age, current health status, motivation, and lifestyle.
“There is a wide spectrum of treatments,” Ruckle says. “It is really important that patients understand that it is not a one-size-fits-all treatment by any means.” Different prostate cancer treatments bear various side effects — from close observation with deferred treatment if necessary, focal therapy to radiation therapies (including proton) to robotic surgical removal.
“We have a lot of resources and options to help men get through this and not have it adversely affect their life or their lifestyle,” Ruckle says.
Get our newsletter for cancer-fighting tips, activities and recipes.
Experts at Loma Linda University Health are committed to providing compassionate, comprehensive, and personalized care along every step of your prostate cancer screening journey. Learn more about prostate cancer screening and treatment options online or call 909-558-6600.
