Previously diagnosed inoperable tumors can be treated with a LITT procedure
Inoperable brain tumors are a diagnosis of the past.
Loma Linda University Health is currently the only center in the Inland Empire offering laser interstitial thermal therapy (LITT), a minimally invasive procedure that allows neurosurgeons to treat tumors once considered unreachable.
Tumors buried deep within the brain, such as those in the thalamus or basal ganglia, often leave patients with few options beyond biopsy, radiation, or comfort-focused care due to the serious risks posed by traditional surgery.
However, using advanced robotics, real-time MRI guidance, and targeted laser energy, physicians can precisely destroy tumor tissue through an incision smaller than a centimeter in a minimally invasive, outpatient surgery.
According to Zachary Gersey, MD, MS, neurosurgeon and LITT specialist, the success of LITT has changed the way brain tumors are viewed, making the term “inoperable” increasingly outdated.
“The data show that LITT is safe, improves quality of life, and may improve overall survival or progression-free survival for certain tumors,” Gersey says.
What is laser interstitial thermal therapy?
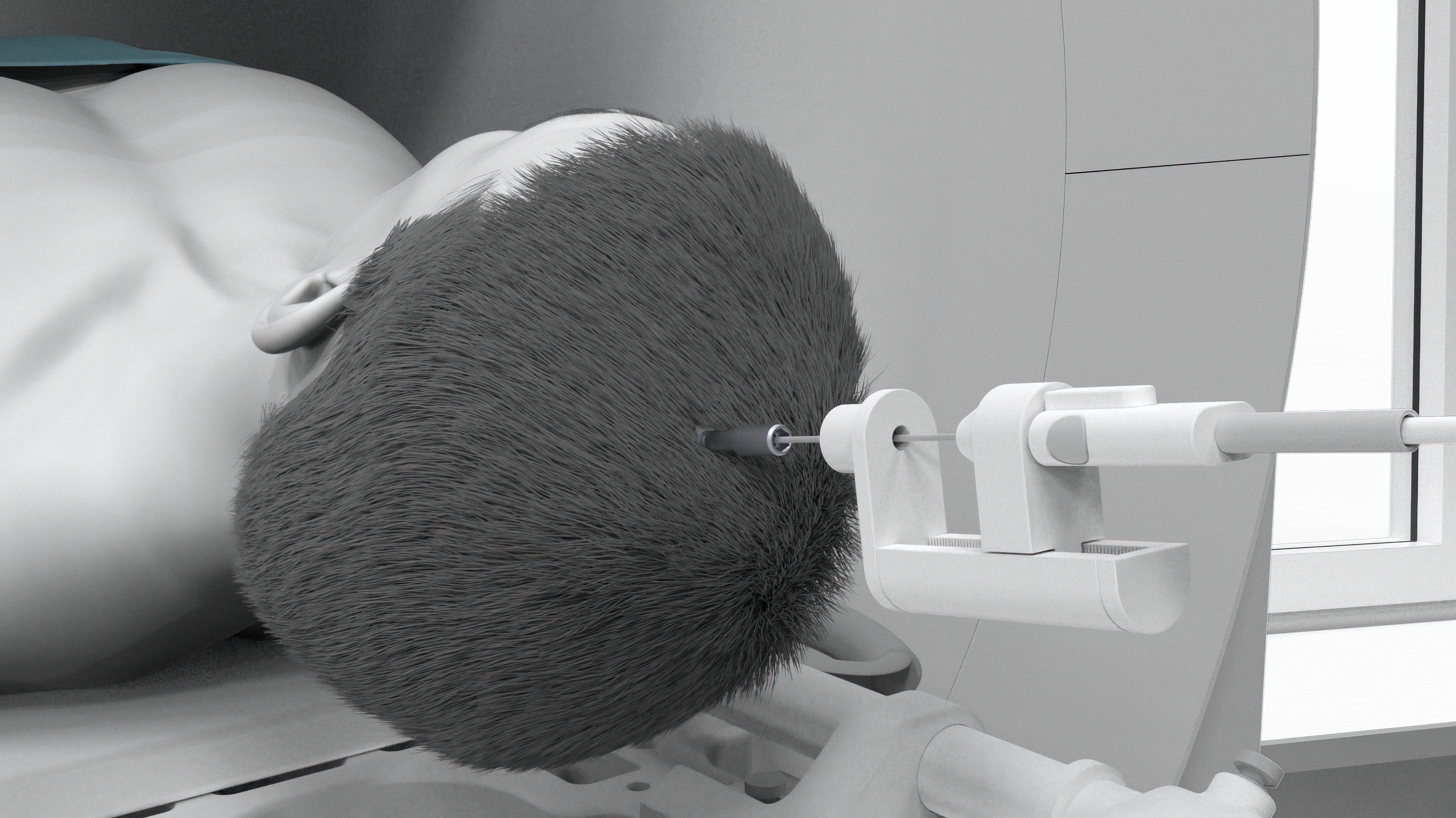
LITT, sometimes called “laser ablation,” is a technique that uses controlled heat to destroy abnormal brain tissue. The procedure is performed using the ROSA robotic system, which allows for sub-millimeter accuracy when placing a catheter with a precise trajectory and depth needed to safely reach the tumor.
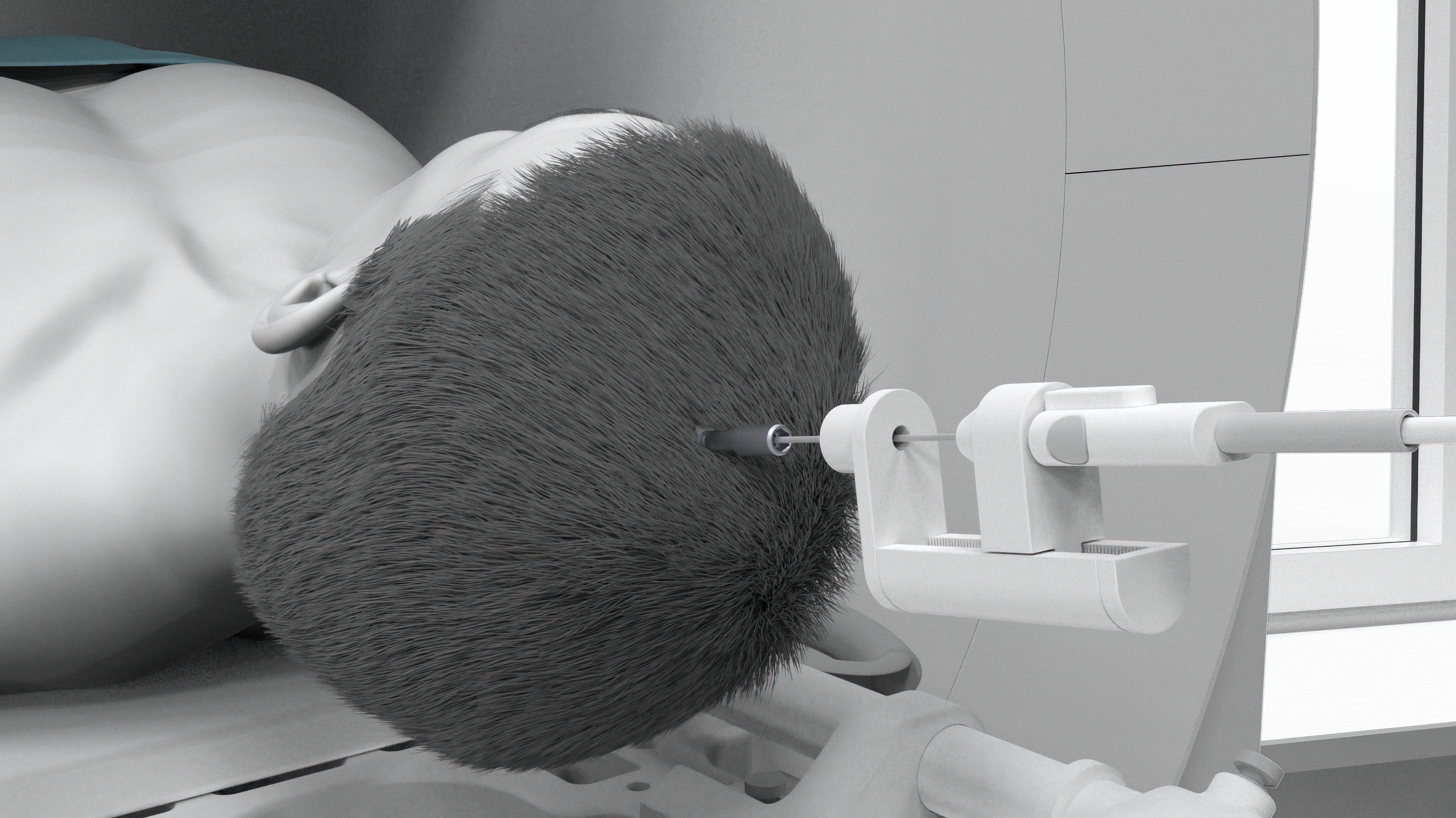
Once the trajectory is set, the ROSA robot guides placement of the LITT catheter, which has a specialized tip that heats up to thermally damage the tumor and surrounding targeted tissue.
After bolt placement in the operating room, the patient is taken to an MRI suite, where another robotic system ensures the device is positioned exactly where it needs to be within the brain.
“During the ablation, surgeons monitor the temperature in real time through MRI imaging, allowing them to see exactly how the heat is affecting the tumor,” Gersey explains. “If critical structures are nearby, the system can limit or block heat from spreading into those areas. Should temperatures rise too high, the system will automatically shut down.”

Because the approach is minimally invasive, recovery is typically quick. Many patients can go home the same day or the day after the procedure.
Treating tumors once considered “inoperable”
Traditionally, the term “inoperable” referred largely to tumor location, where open brain surgery could result in paralysis, coma, or death. While open brain surgery remains the standard, in cases where surgery is deemed too dangerous, laser ablation becomes the preferred surgical method, especially when:
-
The tumor is located in a high-risk or deep-brain area
-
Only part of the tumor can be safely removed
-
The tumor recurs in a dangerous location
-
The patient’s overall health may not tolerate a major operation
-
The patient has radiation necrosis: a treatment-related reaction that can mimic tumor regrowth
In some cases, surgeons can perform a biopsy and ablation during the same procedure, eliminating the need for multiple surgeries.
For patient, Dale Strasshofer, who was diagnosed with radiation necrosis, a serious complication caused by damaged blood vessels, leading to tissue death and edema, undergoing open brain surgery was deemed too dangerous. Instead, Strasshofer received a ROSA-assisted stereotactic needle biopsy and LITT, which not only confirmed the diagnosis but also addressed the lesion at the same time.
“The procedure allowed for a biopsy, a definitive diagnosis, and ablation of the lesion,” Strasshofer said, reflecting on his experience. “I didn’t suffer any side effects, and I had a short, uneventful recovery.”
Recovery and quality of life
Most LITT procedures take approximately three to four hours from start to finish, with patients returning to normal daily activities the same day.
Over time, as the ablated tumor tissue dies and is gradually cleared by the body, swelling decreases, and pressure on surrounding brain structures is relieved.
“If you take away what’s pressing on the brain, function improves,” Gersey explains. “This reduction leads to improvement in symptoms such as weakness, speech difficulty, or cognitive changes.”
While ongoing studies continue to compare laser ablation with traditional tumor removal, current evidence shows that LITT may improve progression-free survival and overall outcomes compared to no surgery or performing a biopsy alone.
“Because of tools like LITT, the term ‘inoperable brain tumor’ shouldn’t be used anymore. There is almost always something we can do surgically,” Gersey says.
For more information about the LITT procedure, contact us at 877-558-0800 or visit our website here.



